Transanal Irrigation (TAI) is known to be a successful therapy to treat LARS, and in this study, Orlandi et al explore the use of TAI as a treatment option for women with endometriosis who experience LARS-like symptoms.
Introduction to the study
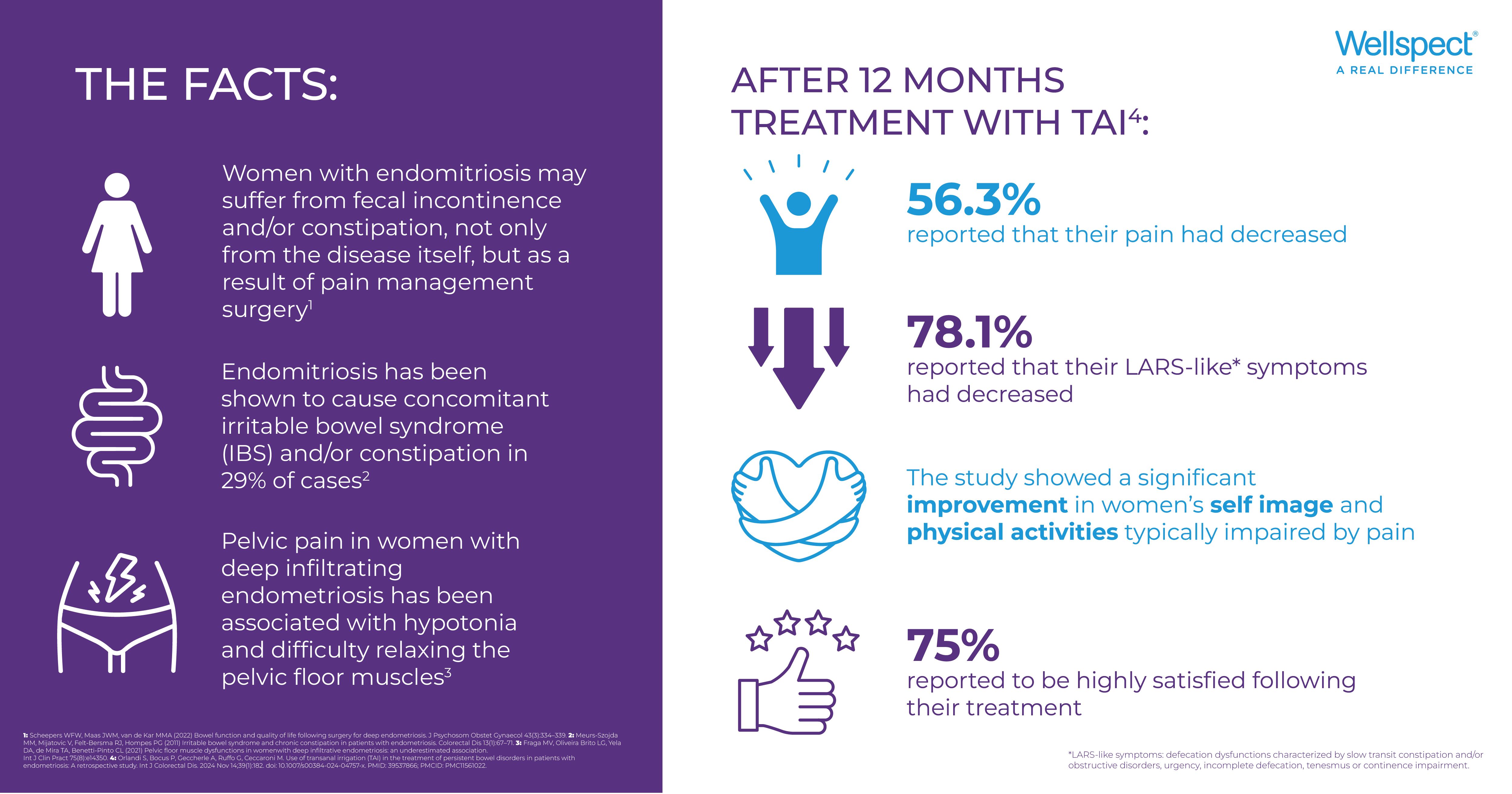
Endometriosis, a chronic inflammatory disease which leads to the formation of endometriotic lesions1, affects approximately 10% of women of reproductive age according to the WHO2. The women affected experience severely debilitating symptoms which have a strong impact on their quality of life (QoL)3. Pain is the main symptom, but 29% of women also experience concomitant irritable bowel syndrome (IBS) and/or constipation4. These bowel dysfunctions present with similar symptoms as patients who experience Low Anterior Resection Syndrome (LARS). Transanal Irrigation (TAI) is known to be a successful therapy to treat LARS5,6, and in this study, Orlandi et al explore the use of TAI as a treatment option for women with endometriosis who experience LARS-like symptoms.
Does endometriosis cause bowel problems?
Pelvic pain in women with deep infiltrating endometriosis (lesions > 5mm deep) has been associated with hypertonia and difficulty relaxing the pelvic floor muscles (PFM). This is thought to be an underlying cause of endometriosis related bowel symptoms7.
Endometriosis is a complex condition, with various treatment approaches including pharmacological and surgical therapies. Most guidelines agree that the use of progestogens and combined oral contraceptives should be used as first-line therapy, but in advanced cases, surgical removal of the endometriotic areas may be needed8.
While surgical intervention may have positive outcomes on pain, this can be offset by various postoperative complications, including LARS-like symptoms9.
Women with endometriosis may therefore suffer from fecal incontinence and/or constipation not only from the condition itself and its effect on the pelvic floor muscles, but also as a result of pain management surgery10.
How to manage bowel problems related to endometriosis?
Endometriosis-related bowel symptoms are poorly understood and lack guidelines and clinical evidence for treatment strategies.
With this study, Orlandi et al point out the symptomatic synergies between patients with LARS and patients with endometriosis-related bowel dysfunction and explore whether the beneficial effects of TAI for treating LARS may translate to the LARS-like symptoms caused by endometriosis.
TAI is a minimally invasive therapy which uses only lukewarm water to irrigate the rectum and colon via the anus, in order to initate peristalsis and expel stool. Regular use of TAI has been shown to reduce constipation, episodes of fecal incontinence and pain caused by bowel dysfunction and as a result improve the patients QoL5.
With the strategy to reduce pelvic floor stress and facilitate rehabilitation, this study aimed to evaluate the effectiveness of TAI in improving pain-related symptoms and QoL of patients with endometriosis and bowel dysfynction.
60 patients who met the inclusion criteria: over 18 years; diagnosed with endometriosis; and presence of bowel symptoms such as urge incontinence, constipation and voiding difficulties participated in the study and were subjected to a pretreatment visit (baseline) to record medical history, pain and satisfaction levels using a visual analog scale (VAS), the Endometriosis Health Profile (EHP)-5 score as well as assesment of LARS-like symptoms using the LARS score.
Is TAI a treatment option for endometriosis-related bowel symptoms?
When comparing baseline data to the results at 12-month follow-up with TAI, Orlandi et al reported the following:
With 32 patients completing the questionnaire at follow up, 75% of patients reported that they were highly satisfied with treatment after 12 months of using TAI. 56.3% reported that their pain had decreased and 78.1% reported a decrease of their LARS-like symptoms. An additional analysis was also performed to evaluate impact of any prior surgery on the outcomes, but no statistical significance was noted. Furthermore, an improvement in the patients’ QoL was also observed as well as a significant change in the patients results in the EHP-5 questionnaire. 40% of patients changed their response to EHP-5 (1) question “Do you find it difficult to walk because of the pain” from “often/always” to “never/rarely” and 35% to “sometimes”.
In response to the question “Do you feel that your appearance has been affected?” EHP-5 (5), 83.3% of patients changed their answer from “sometimes” at baseline to “never/rarely” at follow up, and 31.6% changed from “often/always” to “never/rarely” at follow up.
The weighted kappa statistic indicated that these changes were due to the clinical benefits of the treatment, with correlation observed between changes in QoL and the use of TAI.
Reduced LARS-score
Literature observes that TAI has a positive impact on the QoL of patients with LARS and functional bowel disorders5, which is consistent with the positive results observed in this study on daily life and self-perception. Orlandi et al observes that the literature evaulating the efficacy of TAI in the treatment of LARS patients reports LARS scores of around 12.0 after treatment. In this study the mean LARS-score at follow up was 12.7, which falls within the “no LARS” range where few or no symptoms occur.
Is TAI easy to use?
At 12-month follow up, 12 (20%) participants did not complete the final questionnaire, and 16 (26.7%) discontinued the treatment. The reasons for discontinuing treatment with TAI were due to: occurrence of symptoms/complications (n=2; 3.3%), disappearance of symptoms or need for surgery (n=3; 5.0%), ineffectiveness (n=6; 10%), personal resons (n=3; 5.0%) and techincal difficulties (n=2; 3,3%).
According to Orlandi et al., the observed dropout rate in this study (26.7%) aligns with rates reported in recent literature (18% and 23%) looking at TAI as a treatment for LARS symptoms6,11. However, when considering a broader range of studies, dropout rates for TAI are often reported to be higher, generally falling within the 30-50% range12,13. This highlights the variability in adherence depending on patient population, study design, and follow-up duration.
As mentioned, the study observed a 3.3% discontinuation of treatment due to technical difficulties related to the device and 96.3% of patients did not require any assistance to perform the treatment. Basded on these figures, Orlandi et al conclude that TAI is an easy-to-use device for patients with endometriosis and related bowel dysfunction.
Is TAI-treatment time consuming?
The time required for performing TAI can vary widely based on factors such as the device used, the patient's condition, and their experience with the technique. Looking at previous literature, it often appears to be most time cosuming during the initial stages when the patient is learning and adapting the routine to fit their needs. With practice and experience, the time required for TAI tends to decrease13.
For this study, 56% of patients required an average of 30-45 minutes for the procedure, while only 12% required up to one hour. Most patients in this study (60.9%) performed treatment on alternate days (or three times per week) and the mean volume of water used for irrigation was 571ml (+- 237ml).
Does TAI help with endometriosis pain?
Orlandi et al note in their study that the promising results shown for using TAI to treat LARS-like symptoms were also noted in terms of pain relief. Pain relief was observed in more than half the patients, following 12-month use of TAI and could lead to significant improvements in social, occupational and personal status. By using TAI to manage bowel dysfunction, improved pelvic floor rehabilitation was observed. TAI therefore appears to be a valuable strategy for reducing pelvic floor stress, which could explain the associated pain relief.
The conclusion made by the authors were that the results presented in this study support the effectiveness of TAI in improving pain-related symptoms and QoL in patients with endometriosis in combination with bowel dysfunction. Treatment with TAI showed significant improvements in pain relief, LARS-like symptoms, quality of life and satisfaction in both operated and non-operated patients and could therefore be persumed as a valuable strategy for patients with endometriosis and bowel dysfunction to reduce pelvic floor stress.