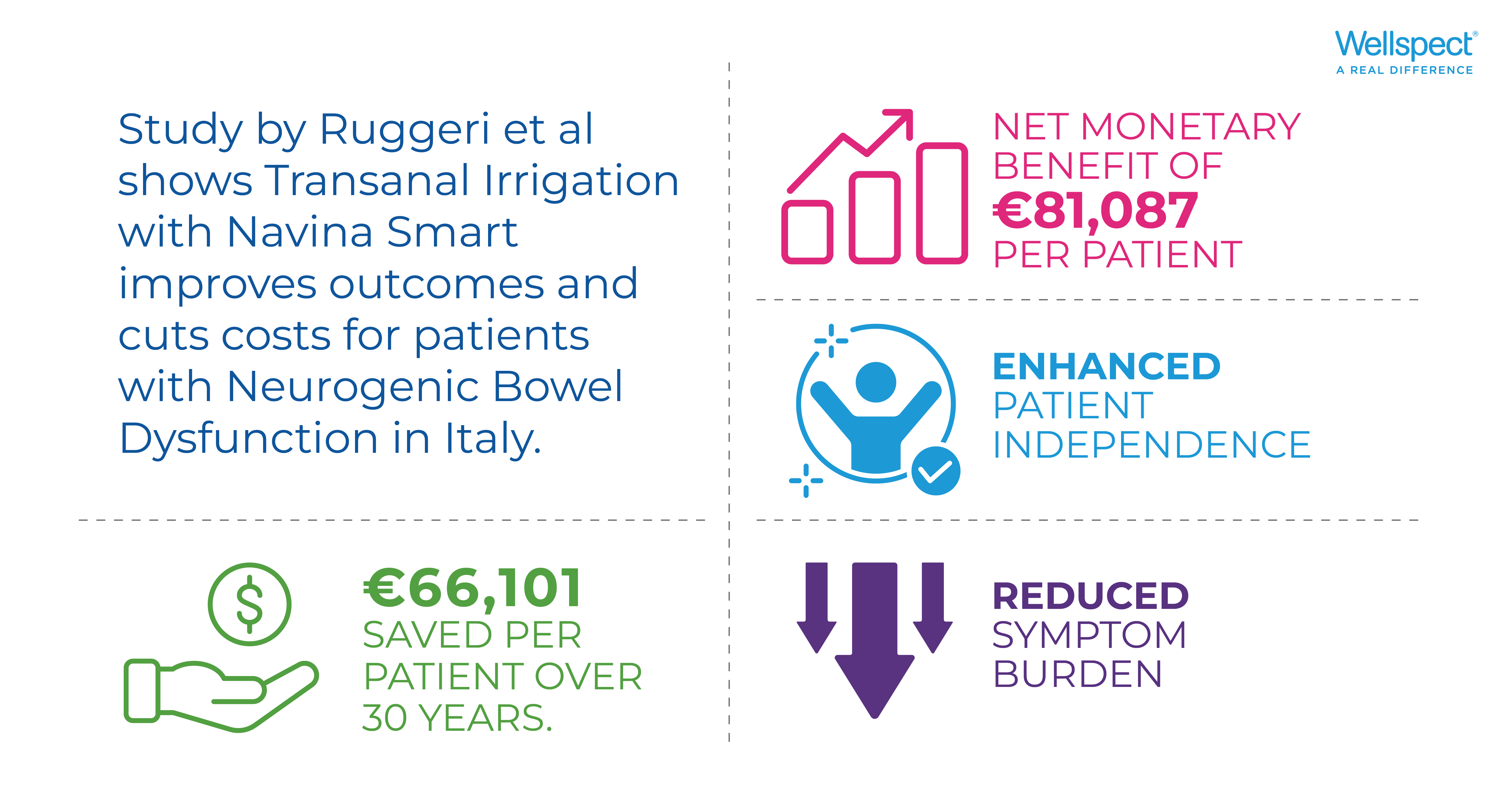
In this study, Ruggeri et al investigated the cost-effectiveness of Transanal Irrigation (TAI) therapy, specifically using the Navina Smart device, for patients with Neurogenic Bowel Dysfunction (NBD) in Italy and compared standard bowel care (SBC) with TAI therapy from an Italian National Health Service perspective.
Introduction
Cost-effectiveness analysis (CEA) has become a key component in valuing new health technologies1, by determining whether a new technology is worth the additional cost to the health and care system under consideration2. Economic models help to understand whether a treatment or therapy is associated with cost savings compared to an alternative intervention or treatment3. Tools such as quality-adjusted life years (QALYs) combine health-related quality of life and quantity of life to measure the value of health outcomes. Ruggeri et al investigated the cost-effectiveness of Transanal Irrigation (TAI) therapy, specifically using the Navina Smart device, for patients with Neurogenic Bowel Dysfunction (NBD) in Italy and compared standard bowel care (SBC) with TAI therapy from an Italian National Health Service perspective.
Neurogenic Bowel dysfunction from a cost-effectiveness perspective
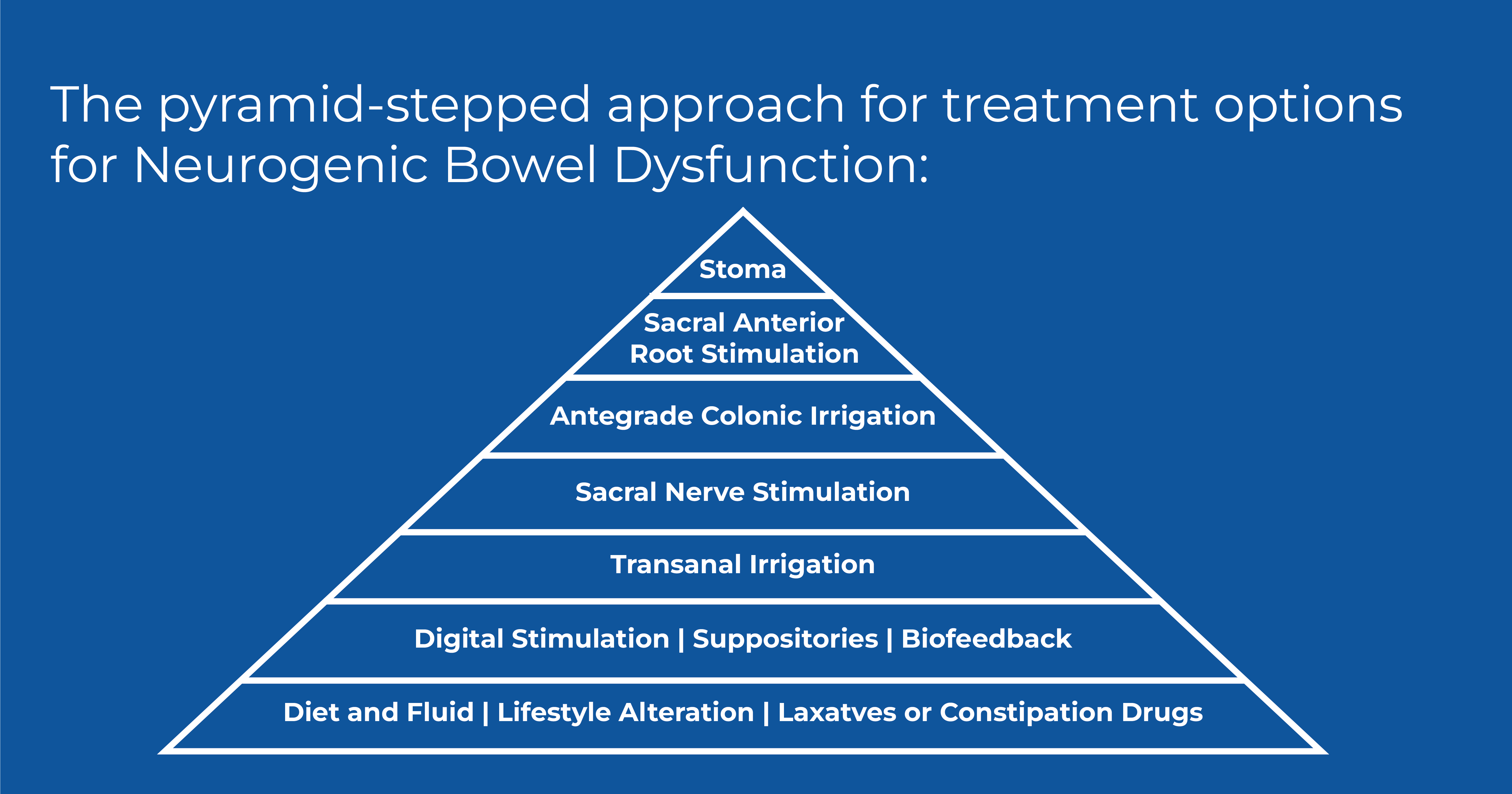
Neurogenic bowel dysfunction (NBD) is characterized by the impairment of normal bowel functions due to a neurological disorder. Symptoms include constipation and fecal incontinence, with the most common complications encompassing urinary tract infections (UTIs), hemorrhoids, abdominal pain, rectal bleeding and prolapse, annal fissure, and autonomic dysreflexia4. These symptoms are commonly associated with recurrent hospital admissions and cause costs related to visits, diagnostic assessments, surgical procedures, and adverse events, such as gastrointestinal infections and intestinal obstructions. Careful evaluation of the patient´s medical history and an accurate clinical examination to determine the most appropriate treatment for each patient is most important. A pyramid-stepped approach for NBD treatment has been extensively used in clinical practice to adapt both the symptoms and the patient´s approach to optimize the patient´s bowel management regimen5. Treatment begins with a conservative approach focusing on optimizing the bowel regime such as SBC and progresses to more invasive measures such as surgical colonic irrigation or the creation of a stoma. There are treatment options in between such as TAI and neuromodulation techniques when SBC treatment is unsuccessful6. Based on this treatment regimen, Ruggeri et al investigated the cost-effectiveness of TAI therapy, specifically using the Navina Smart device, for patients who have failed SBC versus continuing with SBC alone within the Italian context.
Economic model - costs related to SBC and TAI treatment
The cost-effectiveness analysis was conducted using the Markov model. This model allows to systematically evaluate the evolution of a patient´s condition over time. Within this study, Ruggeri et al simulated the different health states that a neurogenic patient can transition between when SBC fails over a 30-year time horizon.
The model simulated on 1-year cycles over a total of 30 years. The transition probabilities related to different patient health states were sourced from the literature. Unit costs related to the treatment of patients receiving SBC and its associated health states were obtained from the Italian National Pharmaceutical Formulary and the Italian Tariff Formulary for outpatient services7,8. Costs associated with TAI treatment (Navina Smart) were provided by the manufacturer Wellspect Healthcare.
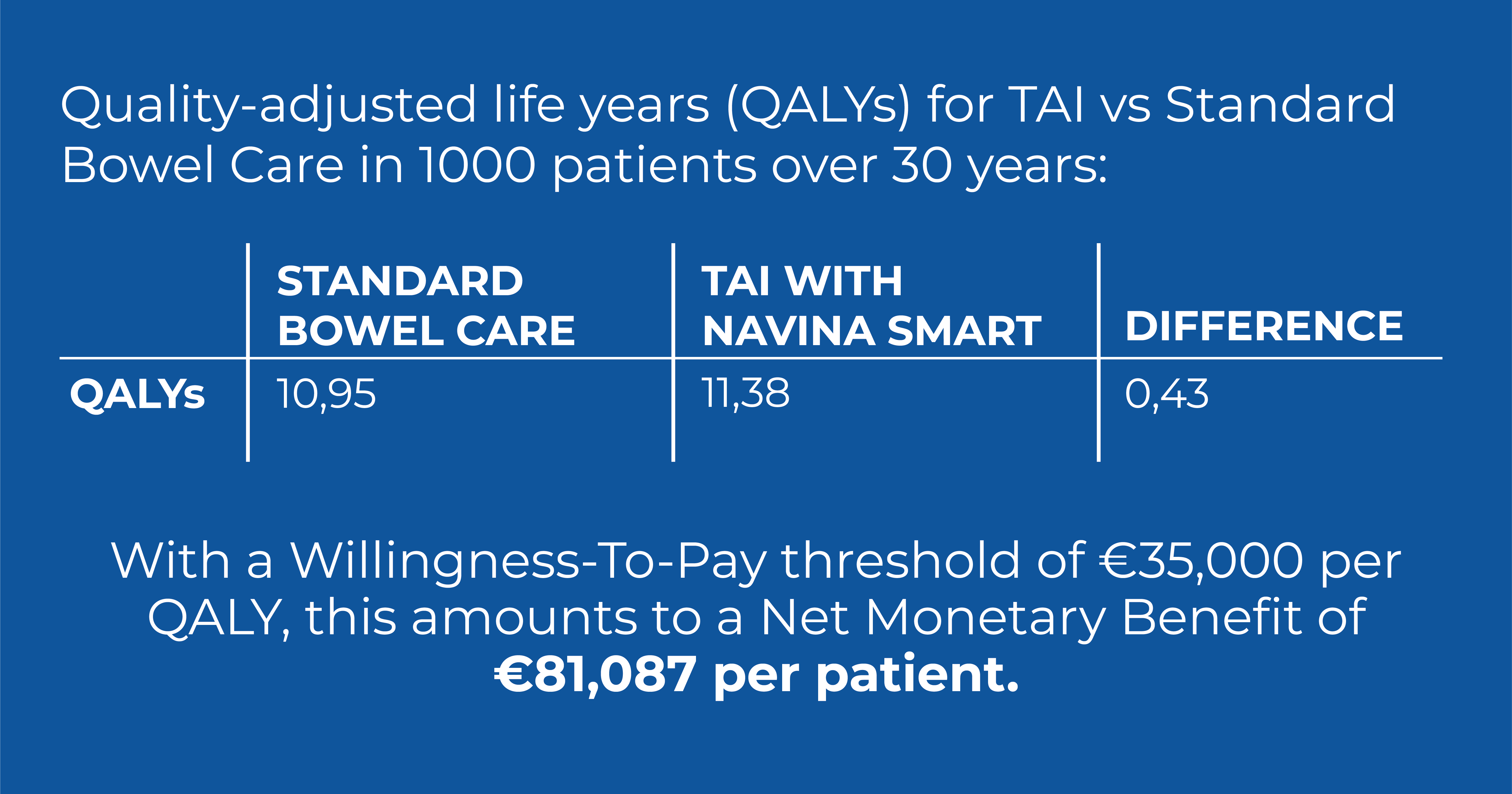
Ruggeri et al compared the costs of the treatment with SBC and TAI in terms of incremental costs and incremental QALYs to indicate that the treatment being analyzed is associated with cost savings compared to the alternative considering a population of 1,000 individuals over a 30-year period. The willingness to pay (WTP) was estimated to be 35,000.00/QUALYs9 (quality-adjusted life years) and is defined as the maximum price or price range that a customer is willing to pay for a product or a service. In addition, the net monetary benefit (NMB) was analyzed to quantify the difference between monetary benefits and associated intervention costs.
The analysis was conducted using a hypothetical population similar to the population described by Emmanuel et al10.
Cost-effectiveness for SBC and TAI treatment
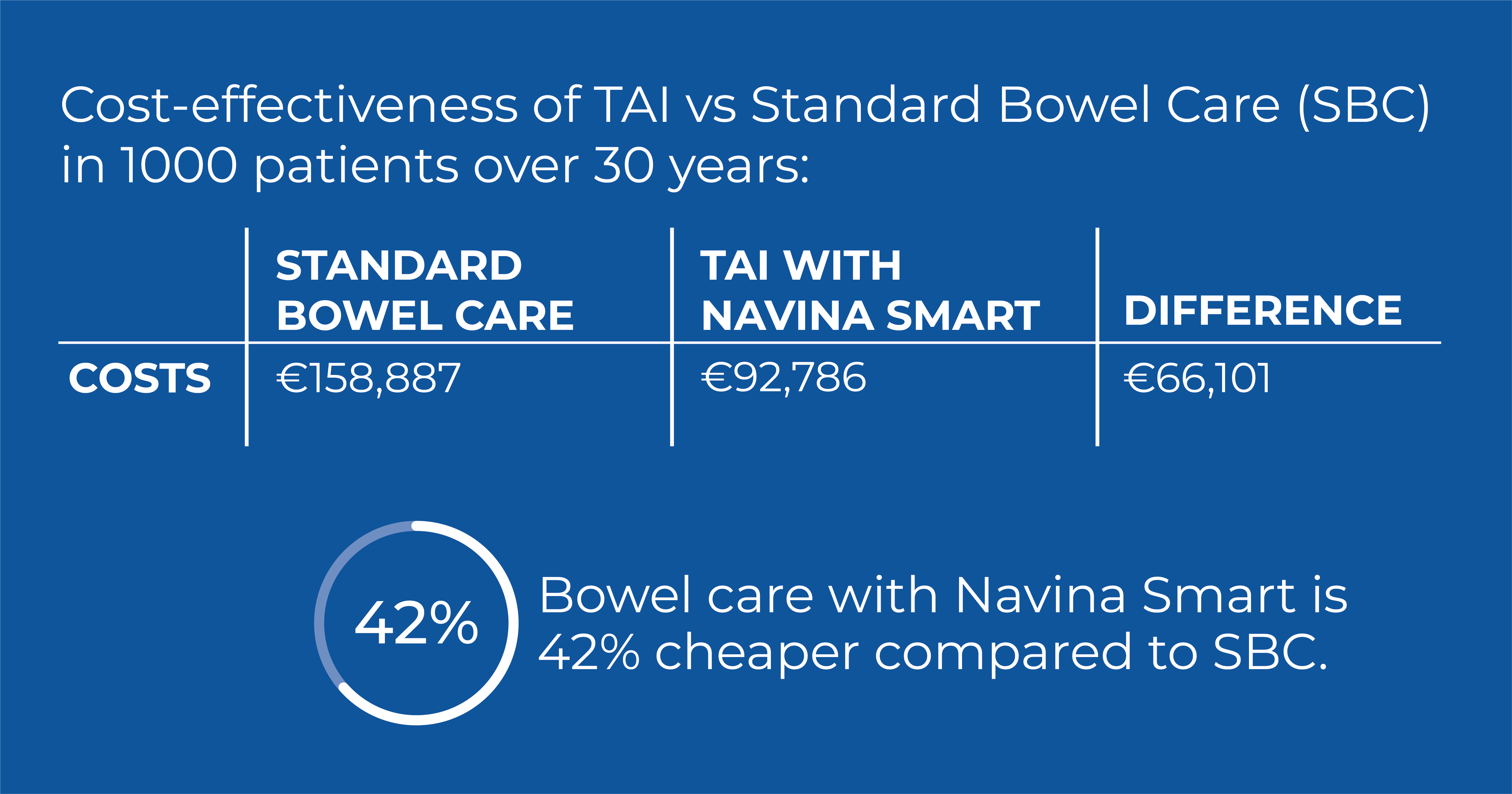
When comparing cost-effectiveness in terms of costs, QALYs, and savings for SBC and TAI treatment over the 30-year time horizon, Ruggeri et al reported the following:
Treatment with TAI was dominant, implying that it was less expensive and resulted in enhanced health outcomes when considering a population of 1,000 individuals over a 30-year period. Notably, the costs associated with SBC exceeded those with TAI.
With a willingness to pay at € 35,000.00/QALYs and comparing incremental costs and incremental QALYs, TAI treatment with Navina Smart has the potential to yield savings of € 66,101 and 0,43 QALYs per patient over 30 years and correlated with reduction in the probability of surgical interventions, stoma creation, adverse events, and HCP visits. The NMB, when quantifying the difference between monetary benefits and associated intervention costs, was estimated to be € 81,087 per patient over 30 years.
Conclusion and study limitations
Ruggeri et al highlighted in their study that Navina Smart TAI for the treatment of NBD shows cost-savings benefits for the Italian NHS compared to SBC treatment. This result was associated with a lower probability of undergoing negative symptoms, visits, and surgical interventions. The results of this analysis can be helpful for decision-makers in the healthcare regulatory and governmental national authorities when allocating scarce resources in national health systems.
The authors pointed out that this model also has some limitations: symptom reduction in severe NBD symptoms, training costs associated with Navina Smart TAI for healthcare staff and patients, and personnel costs and technological equipment were not included in this analysis. The model is simulation-based and provides a hypothetical scenario rather than being grounded on real data and real patients. In addition, the study exclusively compared one second-line alternative (TAI) with SBC and included costs from the British context when the corresponding costs were unavailable in the Italian context.