Publication highlight Ortega et al., Techniques in Coloproctology, 2022
Ortega et al conducted this retrospective study at a pelvic floor disorder center to evaluate the impact of constipation on urogenital symptoms in women. Bowel problems in women are hypothesized to be associated with the presence and severity of urogenital symptoms and linked to pelvic floor dysfunction. Causes of chronic constipation in women vary, but clinical studies show a link to pelvic floor dysfunction, where as many as 50% of people with constipation also have pelvic floor dysfunction. However, it does not show if it is the pelvic floor dysfunction that causes constipation or the opposite. What is known is that bowel emptying and urinary physiology share neural pathways, which explains the co-existence of symptoms.
What are urogenital symptoms?
There are several different urogenital symptoms that can be related to constipation and pelvic floor dysfunction. Stress urinary incontinence, urinary urgency, urinary frequency, nocturia, and urinary hesitancy are commonly reported urinary symptoms. Women with constipation also commonly report dyspareunia (painful intercourse), sensation of incomplete bladder emptying and vaginal splinting (pressing to initiate or complete voiding).
Urogenital symptoms like urinary incontinence, difficulty with bladder emptying, pain, etc, can be evaluated with a validated questionnaire, the UDI-6. This instrument gives a degree of how bothersome the symptom is with a range from 0 to 100, where higher scores indicate more bothersome symptoms.
Constipation in women
Constipation was in this study defined with the Rome IV criteria, where functional constipation is described as experiencing at least two of following symptoms with 25% of bowel movements combined with a decrease in stool frequency:
- Hard stools
- Straining
- Incomplete evacuation sensation
- Use of digital maneuvers
- Sensation of anorectal obstruction or blockage
Constipation is common and more prevalent in women and in individuals older than 65. A way to measure severity of constipation is to use the CSI questionnaire. The CSI score ranges from 0 to 73, where a higher score indicates more severe symptoms. The questionnaire has 3 subscales for obstructive defecation, colonic inertia and a pain scale. In the study summarized here, women were divided into groups based on their constipation symptoms:
- High CSI
- Low CSI
- No constipation
Constipation and urogenital symptoms
Included in the study were 875 women with chronic constipation and 596 women without constipation. The women with chronic constipation were more likely to report:
- Urinary hesitancy
- Sensation of incomplete bladder emptying
- Bladder splinting to complete void
- Dyspareunia
Other symptoms related to constipation was nocturia that was more likely to be reported by constipated women who strained for more than 75% of their bowel movements.
Severity of constipation affects urogenital symptoms
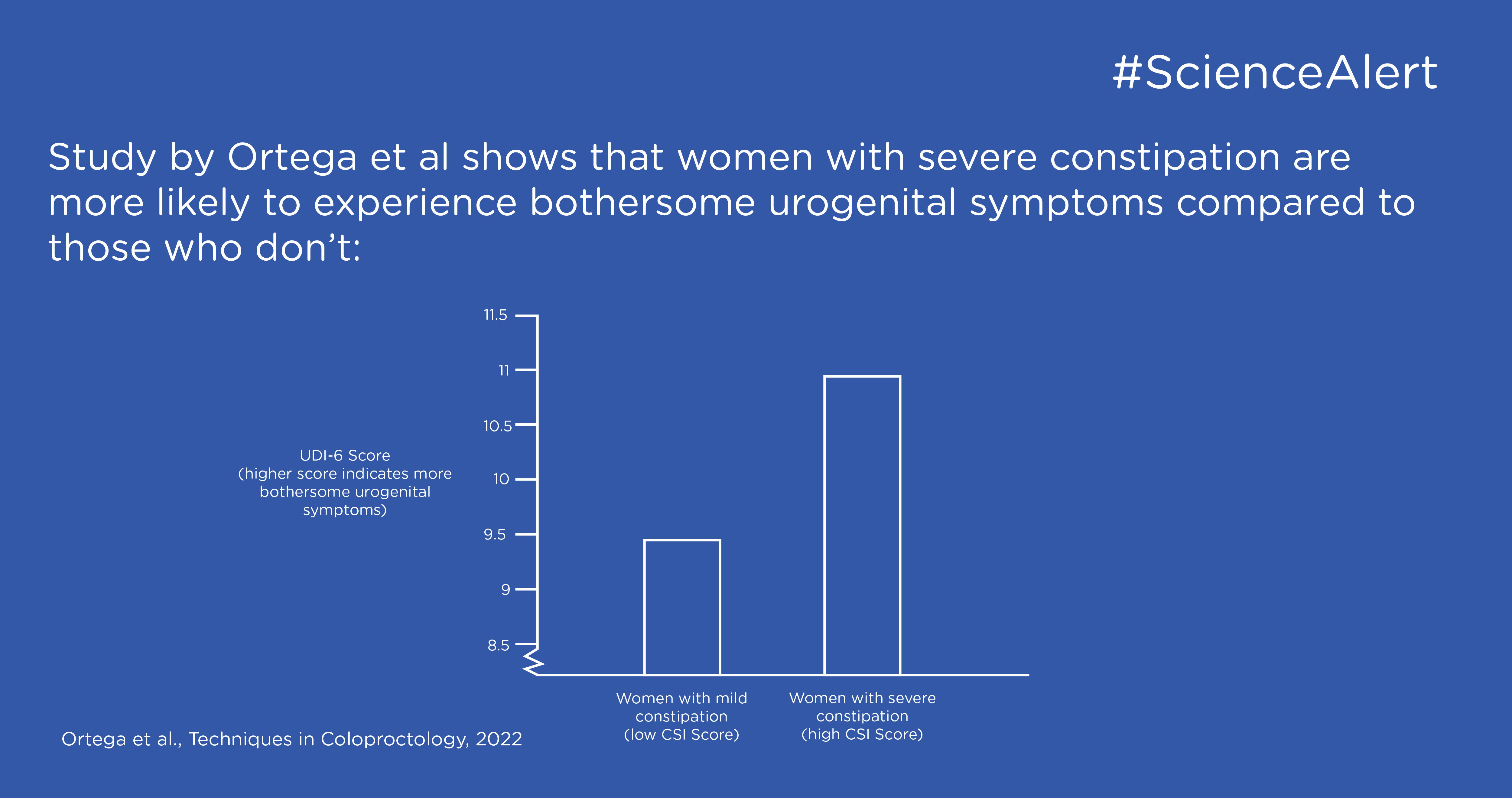
Of the 875 women with constipation, 672 had a low CSI score and 203 had a high CSI score indicating more severe symptoms of constipation. The women with more severe constipation, i.e., the high CSI group, had significantly higher UDI-6 scores meaning that they had more bothersome urogenital symptoms. The women with more severe constipation were also more likely to report bladder splinting and dyspareunia.
The finding that more severe constipation is associated with more severe urogenital symptoms suggest a close association of the symptoms. One weakness in the study was that chronic constipation was not divided into different subtypes, such as functional constipation, slow transit constipation or obstructive defecation. Obstructive defecation is more related to pelvic floor function and a stronger association may be expected in this subtype.
Necessity of a multi-disciplinary approach
The authors conclude that since constipation and severity of constipation affects urogenital symptoms it is important to assess both urogenital and bowel symptoms to provide comprehensive care. This is important to highlight since urinary incontinence is commonly treated with anticholinergic medications that are constipating. Therefore, to improve quality of life for patients with pelvic floor dysfunction a gold standard should be a careful balance of treatments considering all symptoms.