Publication highlight Ethans et al., J Spinal Cord Medicine, 2022
In this publication highlight you can read about how to manage bowel dysfunction in individuals with cauda equina syndrome.
Ethans et al performed this small study to evaluate the efficacy of transanal irrigation (TAI) in people with cauda equina syndrome (CES). They included 12 individuals with CES that used TAI for 10 weeks and evaluated changes in bowel function with the neurogenic bowel dysfunction (NBD) score.
What is cauda equina syndrome?
Cauda equina syndrome (CES) is a spinal cord injury below the conus medullaris, usually in the lumbar spine (L1-L5), compressing or damaging a bundle of nerves called the cauda equina. This typically results in lower motor neuron bowel dysfunction, or areflexic bowel, characterized by:
- loss of peristalsis causing prolonged colonic transit time
- loss of reflex activity causing flaccid anal sphincters
Therefore, symptoms of cauda equina syndrome are constipation, or even severe fecal impaction, and fecal incontinence. In turn, symptoms of constipation and fecal incontinence may lead to additional health problems such as infection of pre-existing pressure injuries or urinary tract infections.
Early symptoms of cauda equina syndrome includes pain radiating to the legs (often misdiagnosed as sciatica) and bladder and bowel dysfunction.
Cauda equina syndrome treatment
One of the highest priorities for individuals with spinal cord injuries are improving bowel function. In guidelines for lower motor neuron bowel dysfunction in CES the aim is to achieve formed and firm stool and then stimulate rectum by manual evacuation and Valsalva maneuvers. However, this bowel management works poorly in people with CES. In the study summarized here, all participants used digital stimulation and manual evacuation, most in conjunction with suppositories, laxatives, or some form of stool softener, at study start.
Transanal irrigation (TAI) is a bowel management method that introduces water to the lower colon through a rectal catheter, which can stimulate colonic peristalsis and soften stool. Many studies have shown that TAI improves symptoms of constipation and fecal incontinence and to be a cost-effective treatment option for neurogenic bowel dysfunction. Ethans et al is the first study publishing results on use of TAI solely in individuals with CES that usually have a flaccid anal sphincter with no or little muscle tonus.
Transanal irrigation as management of cauda equina syndrome bowel dysfunction
The participants included in the study had tried and failed standard bowel management according to Paralyzed Veterans of America (PVA) guidelines, they spent 30 mins or more on bowel management daily or every other day, and had episodes of fecal incontinence once or more per month. At their first visit to the clinic the evaluation of bowel dysfunction showed:
- Mean NBD score as severe 17.9 (0-6 very minor, 7-9 minor, 10-13 moderate, and 14+ severe bowel dysfunction)
- Mean Cleveland constipation score was 18.2 (a score above 15 is considered as constipation)
- Mark’s incontinence score was 15.1 (≥9 indicates significant incontinence)
Each participant was their own control, and the main objective was to compare baseline data to after 10 weeks use of TAI. Participants were instructed in use of TAI with 500-1000 ml of water, to irrigate daily the first 2 weeks and then they could choose to continue with daily irrigations or every other day. During the trial they should not change any medications and they were followed up regularly every week to check on progress. After 10 weeks use of TAI the evaluation of bowel dysfunction showed:
- Mean NBD score as minor 7.8 (0-6 very minor, 7-9 minor, 10-13 moderate, and 14+ severe bowel dysfunction)
- Mean Cleveland constipation score was 12.4 (a score above 15 is considered as constipation)
- Mark’s incontinence score was 11.3 (≥9 indicates significant incontinence)
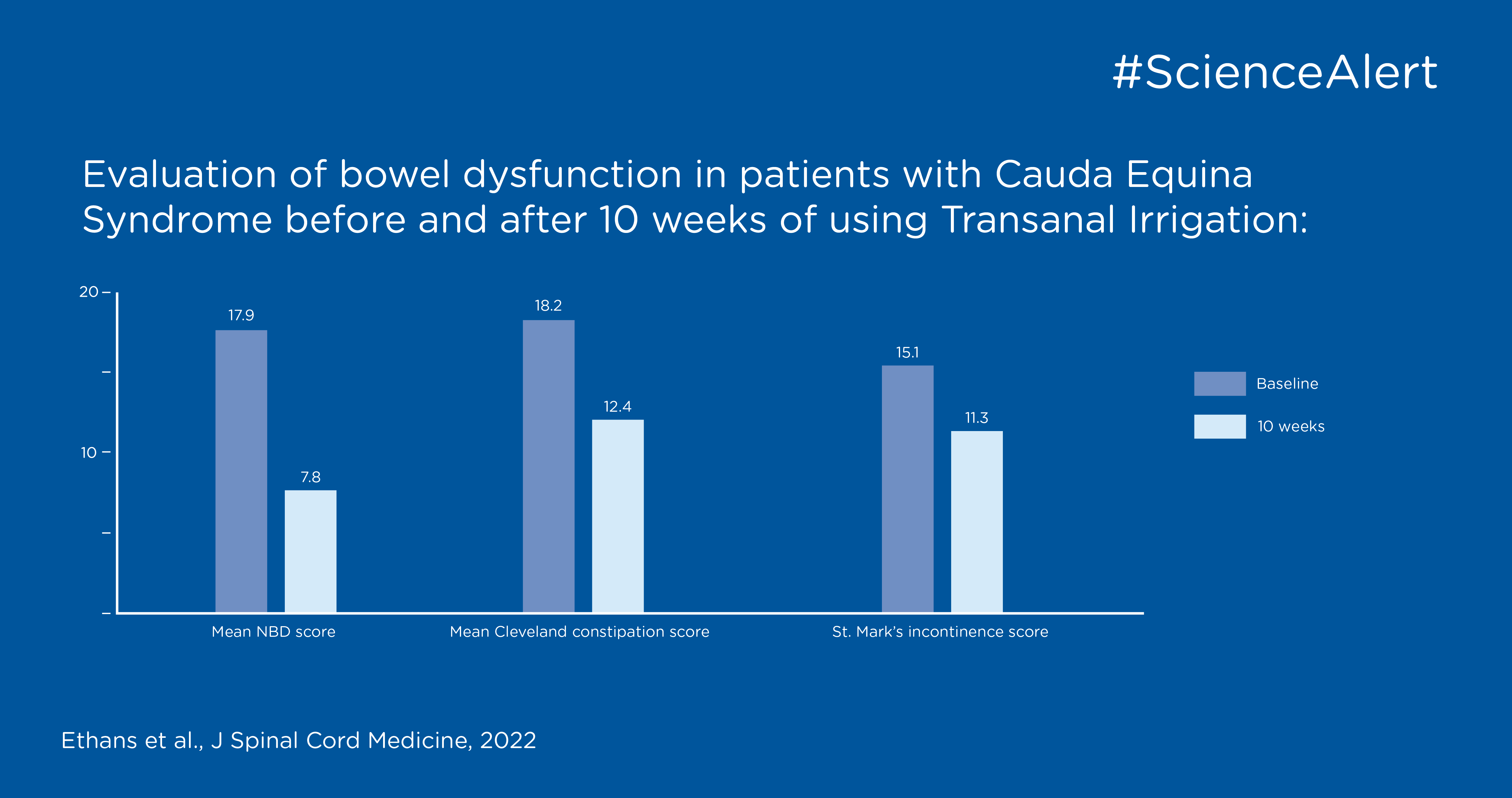
All evaluations showed a clinically relevant and statistically significant improvement of bowel function. There were 2 participants that did not complete the study due to difficulties with the therapy. One had leakage after irrigation, and one had difficulties with using the system as it would fall out of place. Some participants completing the study also had difficulties to keep the catheter with the balloon in place, due to little or no sphincter function. However, they manage to hold the catheter in place with one hand and performing the procedure with the other hand. There was no serious adverse event reported, but a few minor reports of cramping that was resolved with a slower instillation of water.
Living with cauda equina syndrome
Living with cauda equina syndrome and bowel dysfunction often have a negative impact on the individual’s social life and community participation. Using TAI improved the study participants bowel function and to see the impact on their quality of life, the following measures were evaluated:
- the Quality of Life (QOL) score with a max of 52 – higher score meaning better quality of life
- Mean at baseline 25.1
- Mean after 10 weeks use of TAI 35.6
- overall self-rating on a scale from 0-10 (higher equals improvement):
- bowel function had a mean rate of 2.2 at baseline and 5.2 at 10 weeks
- satisfaction with bowel function had a mean rate of 1.6 at baseline and 5.4 at 10 weeks
- influence of bowel function on daily activities had a mean rate of 2.9 at baseline and 6.5 at 10 weeks
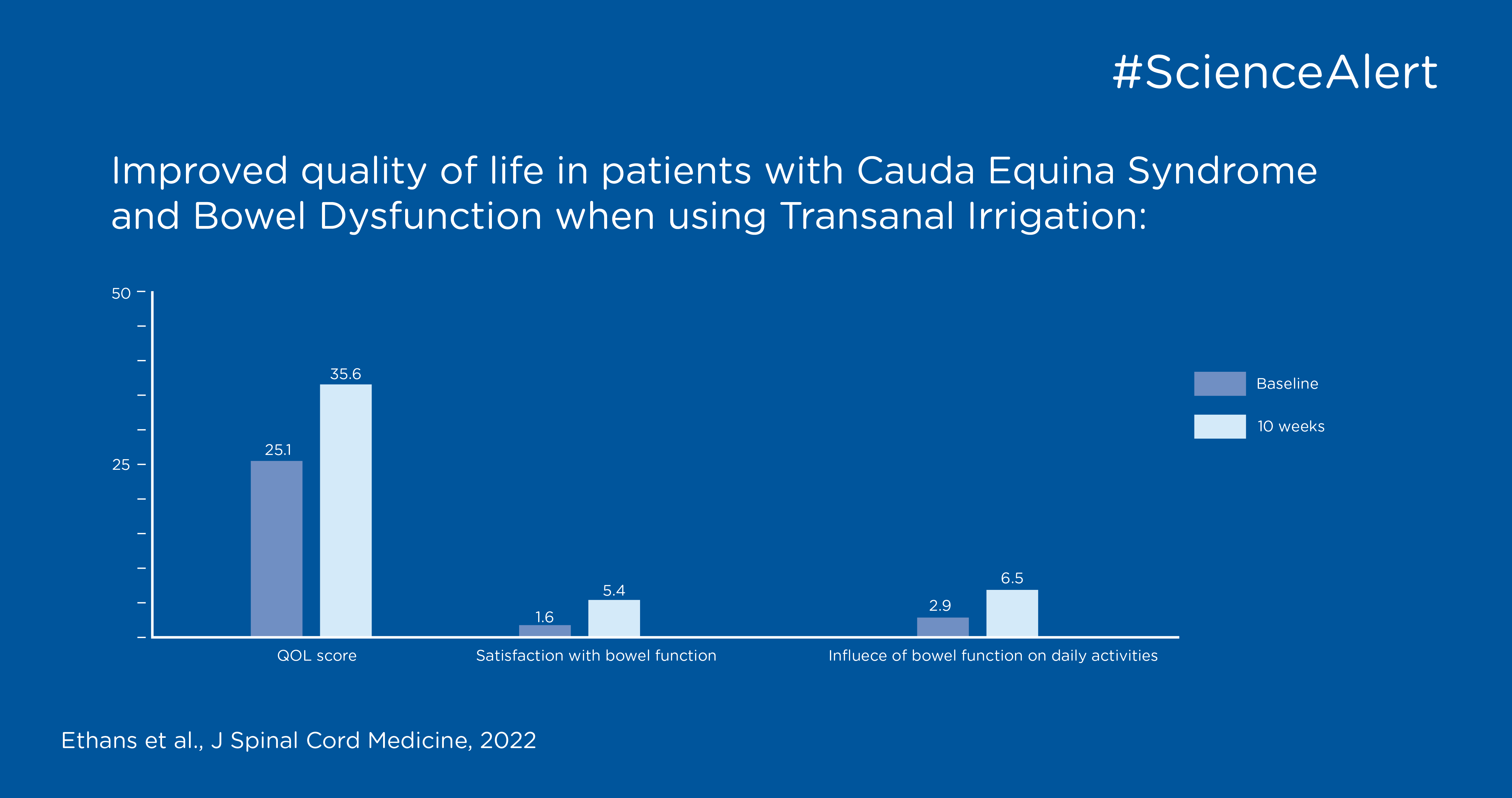
All of the above was significantly improved after 10 weeks use of TAI, which supports the use of TAI in this patient population. The authors conclude that this non-pharmacological bowel management is safe, effective and has the potential to improve the quality of life for patients with CES and neurogenic bowel dysfunction.